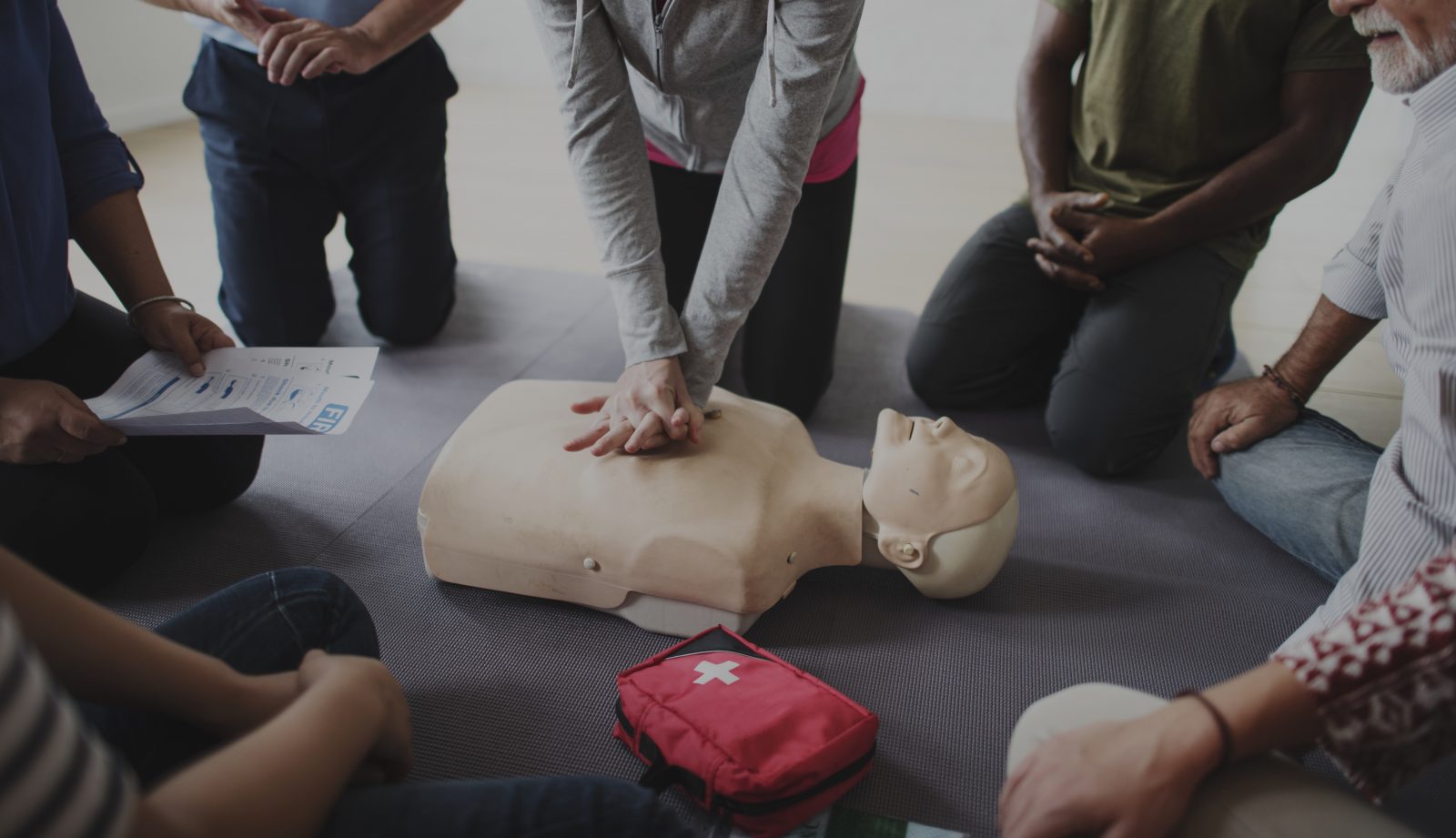
Starbucks barista performs CPR
Natasha Stapp, a barista at Starbucks stepped forward to perform CPR on a stranger when Chris Smith collapsed on the sidewalk out front of the store. “One of the things that I love the most is being able to change somebody’s day,” Stapp said Chris Smith suffered what is nicknamed the Widowmaker Heart Attack. It is a heart problem so deadly, that only about 5% of individuals[..]