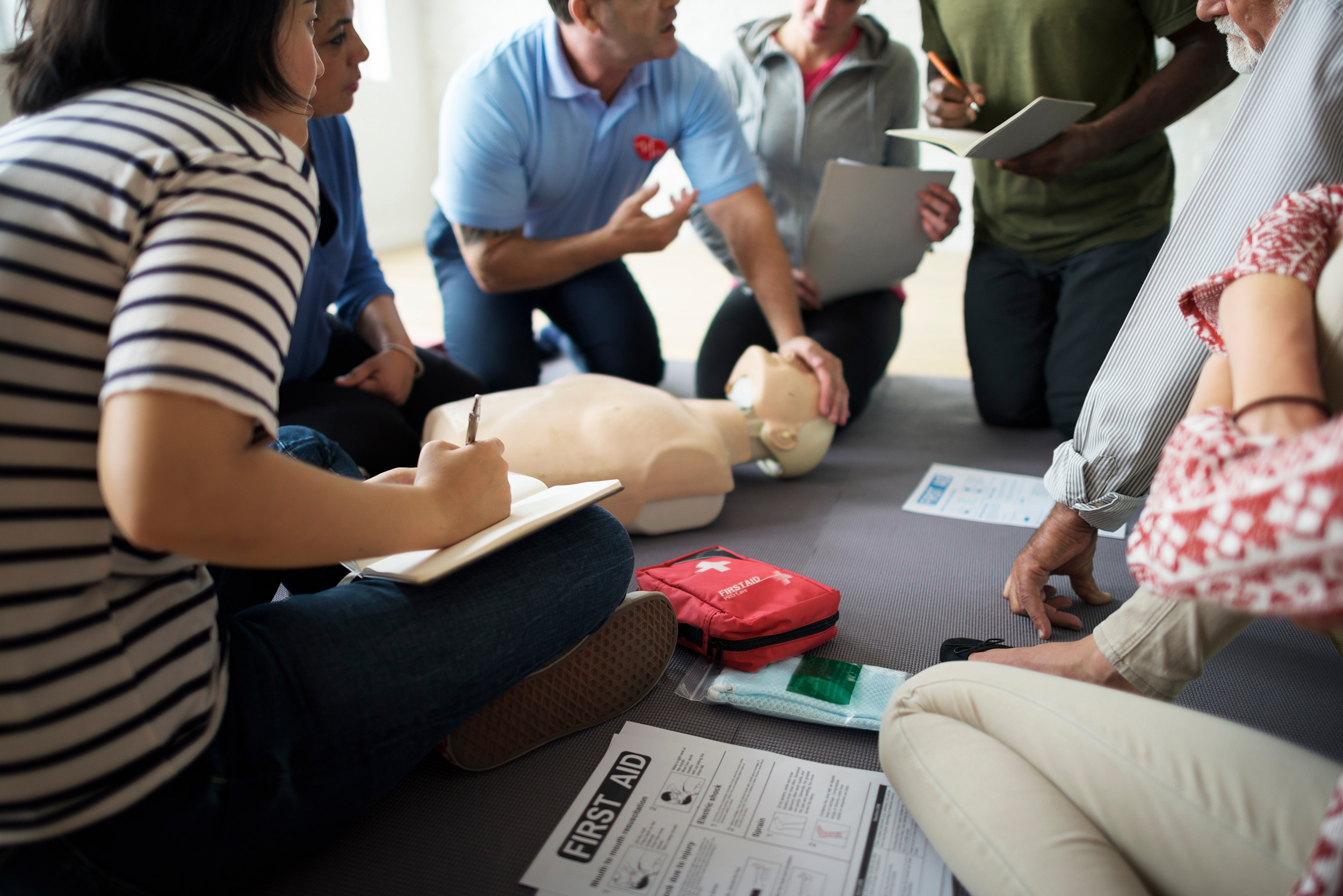
Learn How To Save A Life – First Aid/CPR Classes for Groups & Corporations
CPR/First Aid Training – Corporate and Group Classes UniFirst First Aid + Safety offers weekly CPR classes for companies and groups, UniFirst First Aid + Safety’s CPR, AED and First Aid training program will help employers meet OSHA and other federal and state regulatory requirements for training employees how to respond and care for medical emergencies at work. This 2-year[..]








