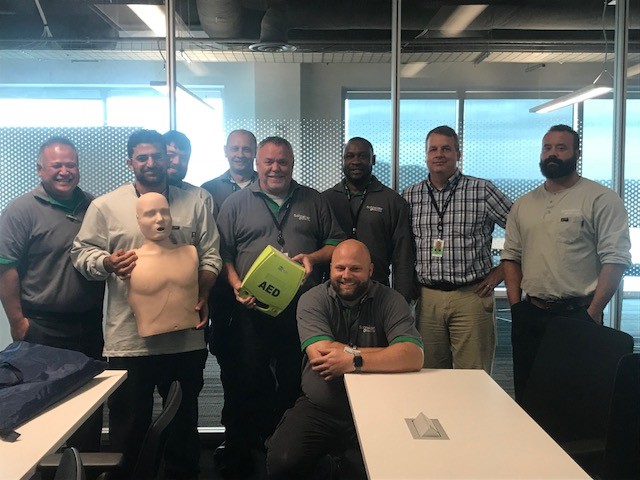
5 Reasons Why Basic First Aid Knowledge Is Important
People often don’t consider the importance of basic first aid education. There are numerous reasons why people put it off.They don’t have the time They don’t know where to begin They don’t believe that accidents will ever happen to them or those close to them They think they already have enough knowledge should the need ariseHelps to save lives.A trained person is more reliable,[..]